Maternity Care Deserts: Bridging the Gaps in Maternal Health
Understanding the Barriers—and How Texas Mothers Can Get Support
Every Texas mother deserves care, no matter her ZIP code.
But for thousands of women, maternity care is too far away, or not available at all. Save Texas Moms is working with partners across the state to close those gaps, one county at a time.
Discover where Maternity Care Deserts exist in Texas, why they matter, and how Save Texas Moms is bridging access gaps through outreach, education, and support.
What Are Maternity Care Deserts?
Maternity Care Deserts are areas where women lack access to essential maternity services—no hospital offering labor and delivery, no birth center, and no obstetric providers such as OB-GYNs, nurse midwives, or maternal-health physicians.
In Texas, many of these medically underserved areas are within a couple of hours from the state’s world-class medical hubs—yet for local moms, that distance means risking severe complications or delayed care.
When Prenatal Care Comes Too Late
From the National Trend to Texas Reality
Across the United States, roughly one in four pregnant women begin prenatal care after the first trimester—a national red flag for maternal and infant health. In Texas, the situation is more urgent. According to the March of Dimes, approximately 20–25% of pregnant women in Texas receive inadequate or no prenatal care, compared to about 15% nationally.
This challenge is compounded by the fact that about half of Texas counties are classified as maternity care deserts, meaning they lack hospitals offering obstetric care and obstetric providers. As a result, pregnant mothers in rural and underserved areas face longer travel times, fewer provider options, and a higher likelihood of delayed or missed prenatal care—conditions that significantly increase the risk of complications for both mother and baby.
Source: March of Dimes, 2023 (PeriStats)
Maternity Care Access Categories
Maternity Care Desert
Counties with no hospitals offering obstetric care, no birth centers, and no obstetric providers, including OB-GYNs or certified nurse-midwives.
Low Access to Maternity Care
Counties with either a limited number of obstetric providers or a hospital or birth center offering obstetric care, but not both.
Moderate Access to Maternity Care
Counties with some obstetric providers and at least one hospital or birth center offering obstetric care, though access may still be limited by distance, capacity, or provider availability.
Full Access to Maternity Care
Counties with adequate numbers of obstetric providers and facilities offering obstetric care provide more consistent and timely access to prenatal, delivery, and postpartum services.
Source: March of Dimes, 2023

The Maternal Health Gaps
Currently, about half of Texas counties are Maternity Care Deserts
1 in 5 Texas moms receive inadequate prenatal care
Right now, 94 rural hospitals have no labor & delivery (L&D) services
The median drive time to a hospital with L&D services is 37 minutes
21 rural hospital closures in the last decade—more than any other state
To date, more than 100 rural hospitals have experienced losses in services
70+ Texas hospitals have closed their labor and delivery units since 2013
These gaps are especially severe in rural East Texas, the Panhandle, and parts of West Texas
Sources: Center for Quality Healthcare & Payment Reform, 2025; Texas DSHS, 2024; The Texas Hospital Association, 2023; March of Dimes, 2023; and Every Texan, 2022
Connectivity Gap in Rural Texas
Many rural Texas communities still lack reliable broadband and telehealth infrastructure—a necessary foundation for prenatal education, remote monitoring, and in-facility coordination.
A Broadband build-out in Texas is behind schedule, with funding and deployment delays reported in 2025.
The federal Rural Health Care Program that supports rural provider connectivity was upheld by the U.S. Supreme Court in June 2025, preserving vital funding for rural healthcare telecom.
At STM, we recognise that both a lack of provider access AND a lack of digital connectivity contribute to Maternity Care Deserts, so we are designing our new SMS service to work even in low-bandwidth settings and to support facilities with connectivity challenges.
More Statewide Support for Moms
Sources: Governing, 2025; Reuters, 2025
Why It’s Happening
Rural Hospital Closures
The reasons are numerous: Low and/or stagnant Medicaid and Medicare payments, increasing operational costs, high rates of uninsured patients, and healthcare staffing shortages have forced publicly funded rural hospitals to struggle.
Insurance Gaps
Texas mothers living in Maternity Care Deserts face limited access to in-network providers, and many insurance plans do not comprehensively cover telehealth services, a key solution for accessing care in rural areas. Having lower insurance coverage and socioeconomic barriers is linked to a higher risk of adverse maternal outcomes.
Workforce Shortages
Unlike urban hospitals, rural hospitals are typically unable to offer competitive staffing salaries. As a result, recruiting and retaining staff become a constant problem. With a shortage of rural physicians, patients are redirected, and hospitals lose funding when they fail to retain patients or have insufficient staff. It’s a vicious cycle.
Transportation & Broadband Issues
Traveling further to attend maternal healthcare appointments increases the likelihood of missed appointments, leading to insufficient care and increased rates of preterm birth. All of which endangers the health of the mother and baby. Despite the viability of telehealth, maintaining consistent access to devices and a reliable broadband connection remains a challenge, especially in the most rural parts of Texas.
Why Official Data Understates the Maternal Health Crisis in Texas
Many commonly cited maternal health statistics rely on lagged, county-level data that does not reflect the rapid changes occurring across Texas.
Official classifications of maternity care access often count whether a hospital or provider exists on paper, but do not capture whether care is actually available, affordable, staffed, or accessible in practice. For a number of years now, Texas has experienced ongoing hospital obstetric unit closures, clinic shutdowns, and physician departures, particularly in rural and underserved communities.
As a result, many counties categorized as having “access” now face unstable or functionally unavailable maternity care. Save Texas Moms uses official data as a baseline while recognizing that the real-world access challenges facing pregnant and postpartum mothers are significantly more severe than published figures suggest.
Who’s Most Impacted
Rural Counties
Rural OB hospital and OB unit closures negatively impact many rural families, but especially racial and ethnic minority groups.
Rural counties experience higher rates of emergency department births and Cesarean births.
Women of Color
Blacks and Latinas are more likely to live in Maternity Care Deserts.
American Indian/Alaska native women are disproportionately affected by maternal and infant mortality and maternity care access.
Lower-Income Families
With limited income and minimal transportation options, women living in Maternity Care Deserts must travel 4.5 times farther than women living in full access areas.
Why We Can’t Rely on Telehealth Alone
Many rural Texas communities still lack reliable broadband or have no service at all.
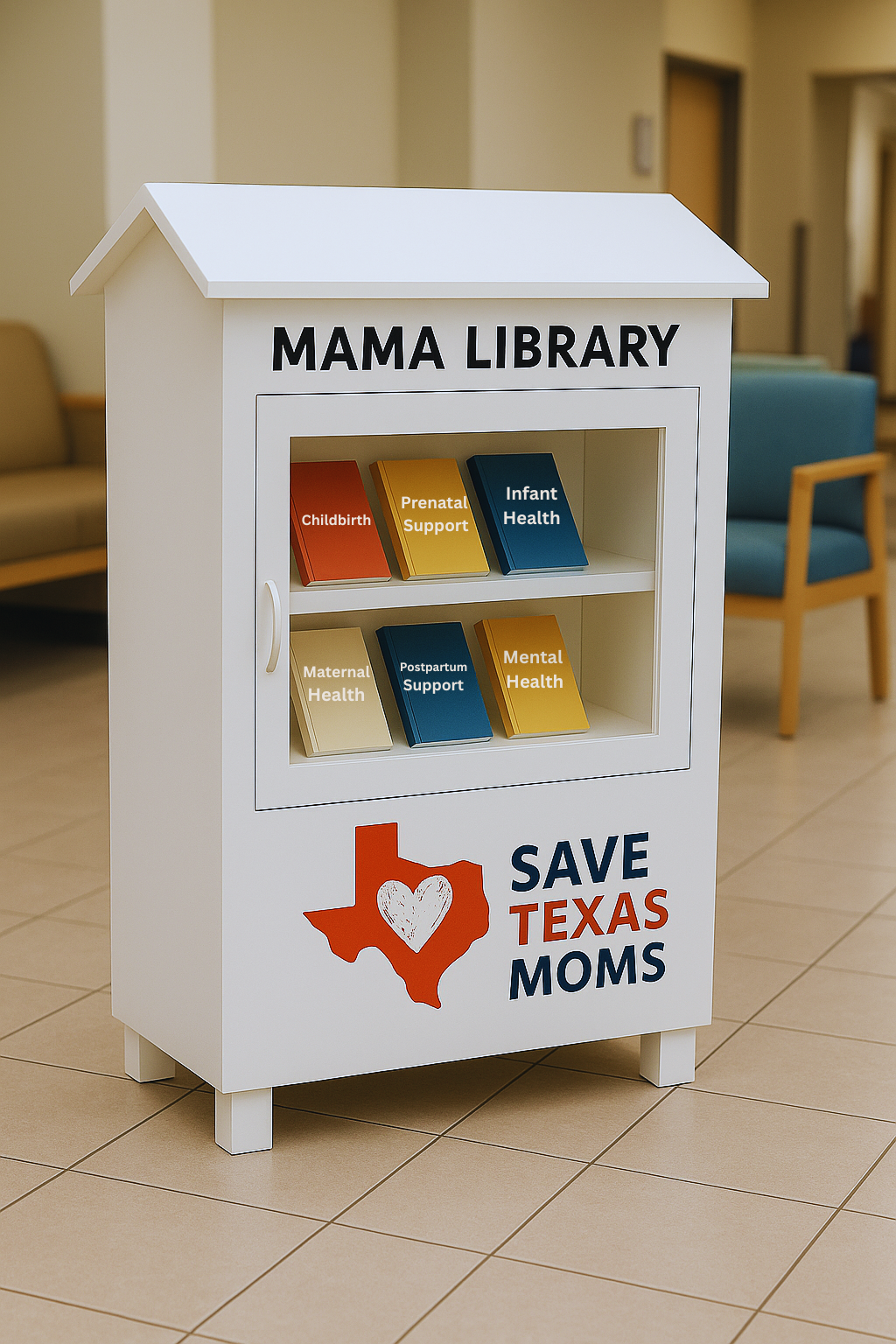
The Mama Libraries will ensure that moms in Maternity Care Deserts can access evidence-based information and local resources—no Internet needed.
Tangible support can save lives.
Want to help us bring a Mama Library to a rural Texas community? Please make a tax-deductible donation.
Why Tangible, Local Support Still Matters
Digital tools and telehealth help to bridge some gaps in rural maternity care, but only when families have the necessary devices and broadband access to utilize them. Many rural Texas communities continue to struggle with inadequate Internet connectivity, high costs, and unreliable coverage. For these mothers, support must also be local, physical, and dependable.
That’s why Save Texas Moms is developing The Mama Libraries for placement across rural regions. These community-based stations provide tangible, no-Internet-needed support, including:
Evidence-based prenatal, pregnancy, and postpartum information
Blood pressure self-monitoring resources
Local referrals to clinics, WIC offices, health departments, and emergency services
Printed materials in English and Spanish
QR codes that work if moms have service—but don’t block access if they don’t
Mama Libraries are designed to meet mothers where they are, even in places where broadband, cell reception, and telehealth still fall short. They are intentionally “Old School”—simple, accessible, physical, and human-centered.
In rural maternity care deserts, tangible support isn’t optional; it’s essential.
Learn more about The Mama Libraries.
How Save Texas Moms Is Closing the Gap
Texts4Moms SMS - With the support of IT partners, we are developing a program to connect rural mothers to real-time support.
The Mama Libraries - We are creating local access points that are convenient and not reliant on the Internet for rural mothers to access information on babies and maternal health.
Data Mapping Internships - We are working with Texas A&M University students in Public Health to map regional resources in Maternity Care Deserts statewide.
Partnership Network - We maintain ongoing collaborations with experts from the American Heart Association, the University of Texas-Tyler, the Houston Health Department, and other organizations to address the maternal health risks faced by rural families.
Please join us as we continue to work toward improving healthcare in Maternity Care Deserts.
Statewide Solutions We Support
The challenges facing Texas mothers in Maternity Care Deserts are not new, and health leaders across the state have been calling for common-sense solutions. The Texas Hospital Association has outlined several approaches that would strengthen maternity care access, especially in rural communities. Save Texas Moms fully supports these recommendations and is committed to advancing them through partnerships and education.
Key recommendations include:
Ensuring sustainable funding for rural hospitals, especially for labor & delivery services that are expensive to staff but essential for community safety.
Improving Medicaid reimbursement rates so that clinics and hospitals can retain maternity providers in underserved regions.
Expanding the rural maternity workforce, including OB/GYNs, family physicians who deliver babies, certified nurse midwives, and labor & delivery nurses.
Investing in telehealth and remote monitoring to connect rural mothers with specialists when local care is limited.
Supporting transportation solutions for families who must travel long distances to reach prenatal or delivery care.
Strengthening partnerships between hospitals, public health departments, and community organizations that provide postpartum support.
STM’s efforts directly align with these statewide priorities and help bring practical support to mothers who are caught in these gaps.